July/August 2013
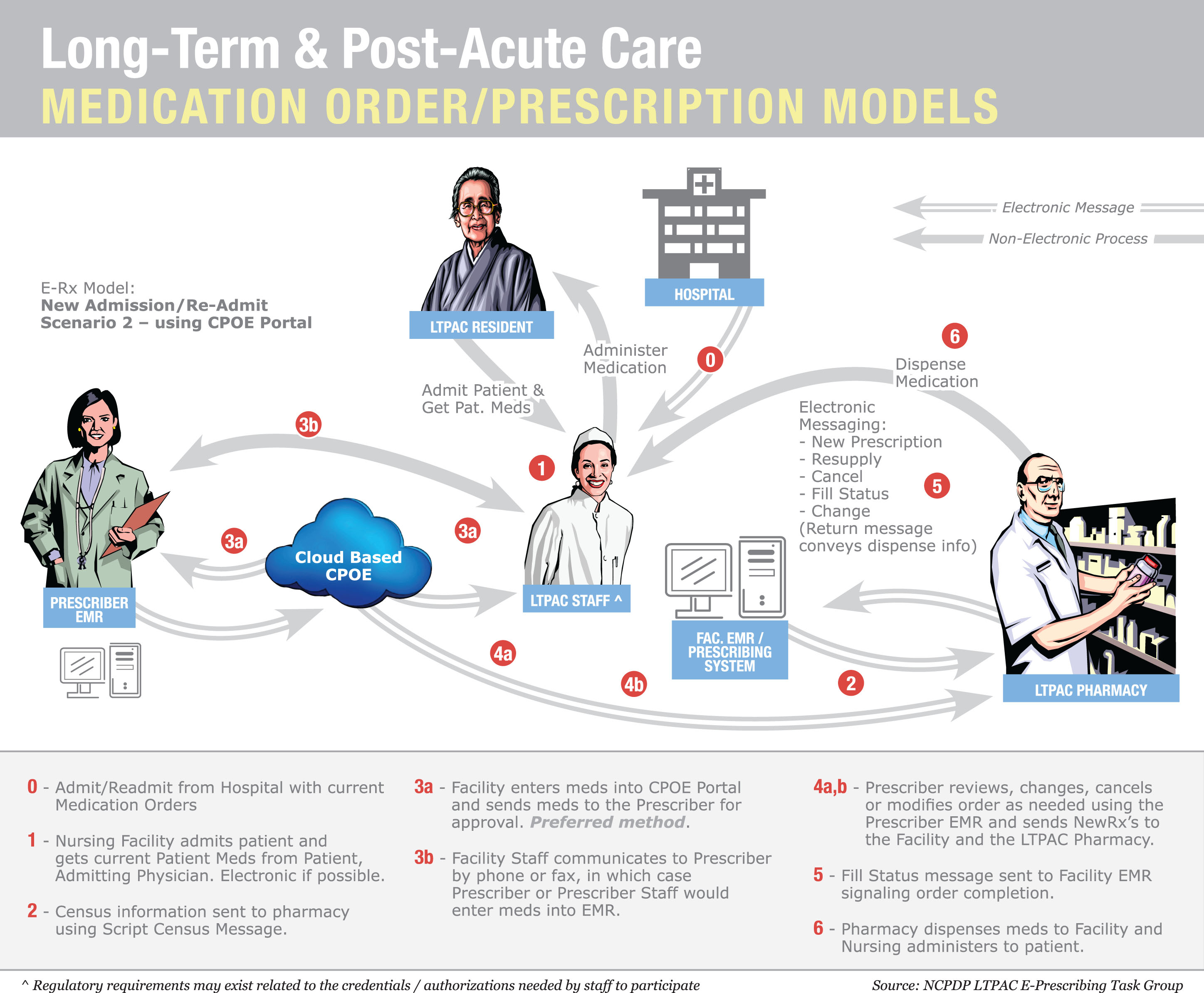
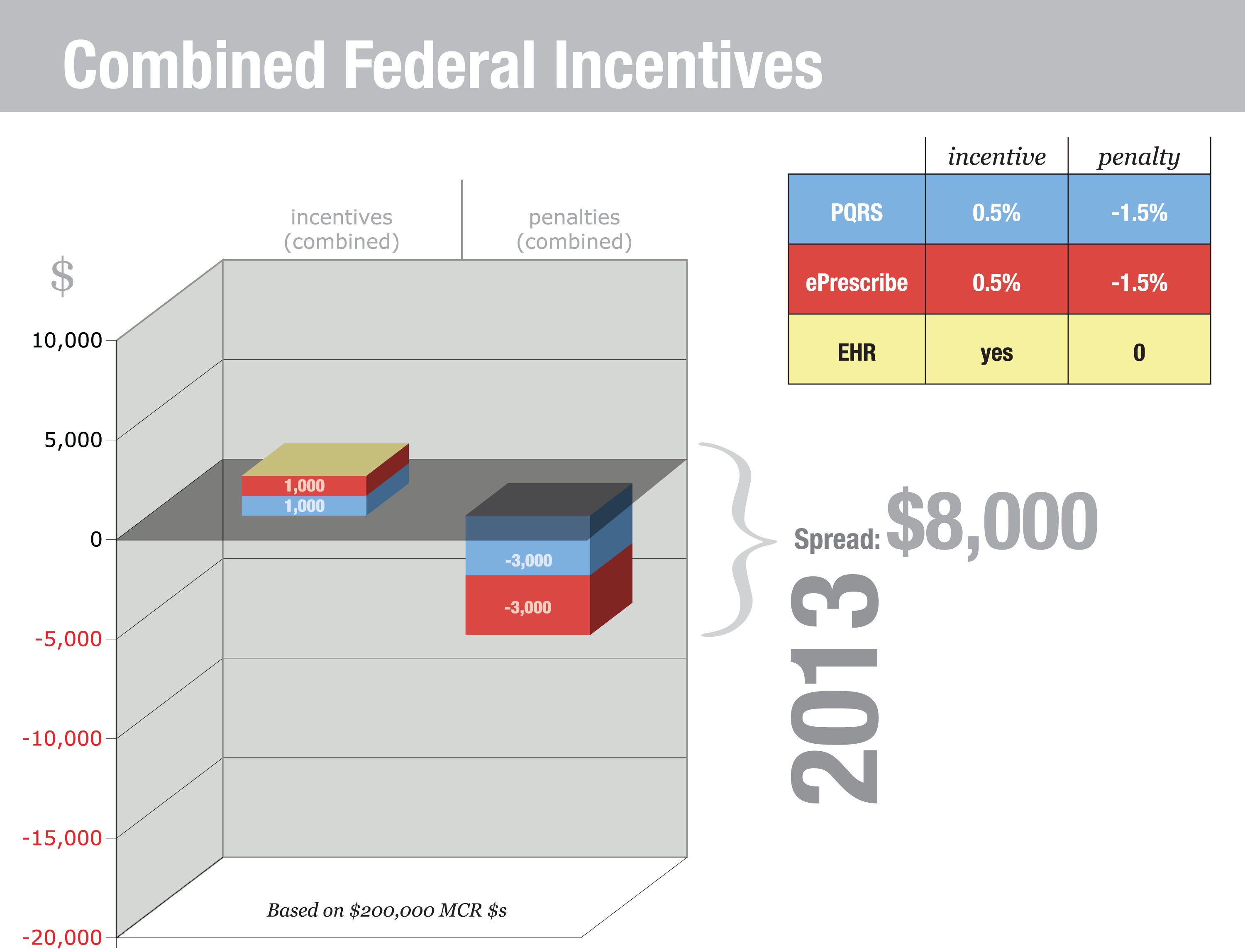
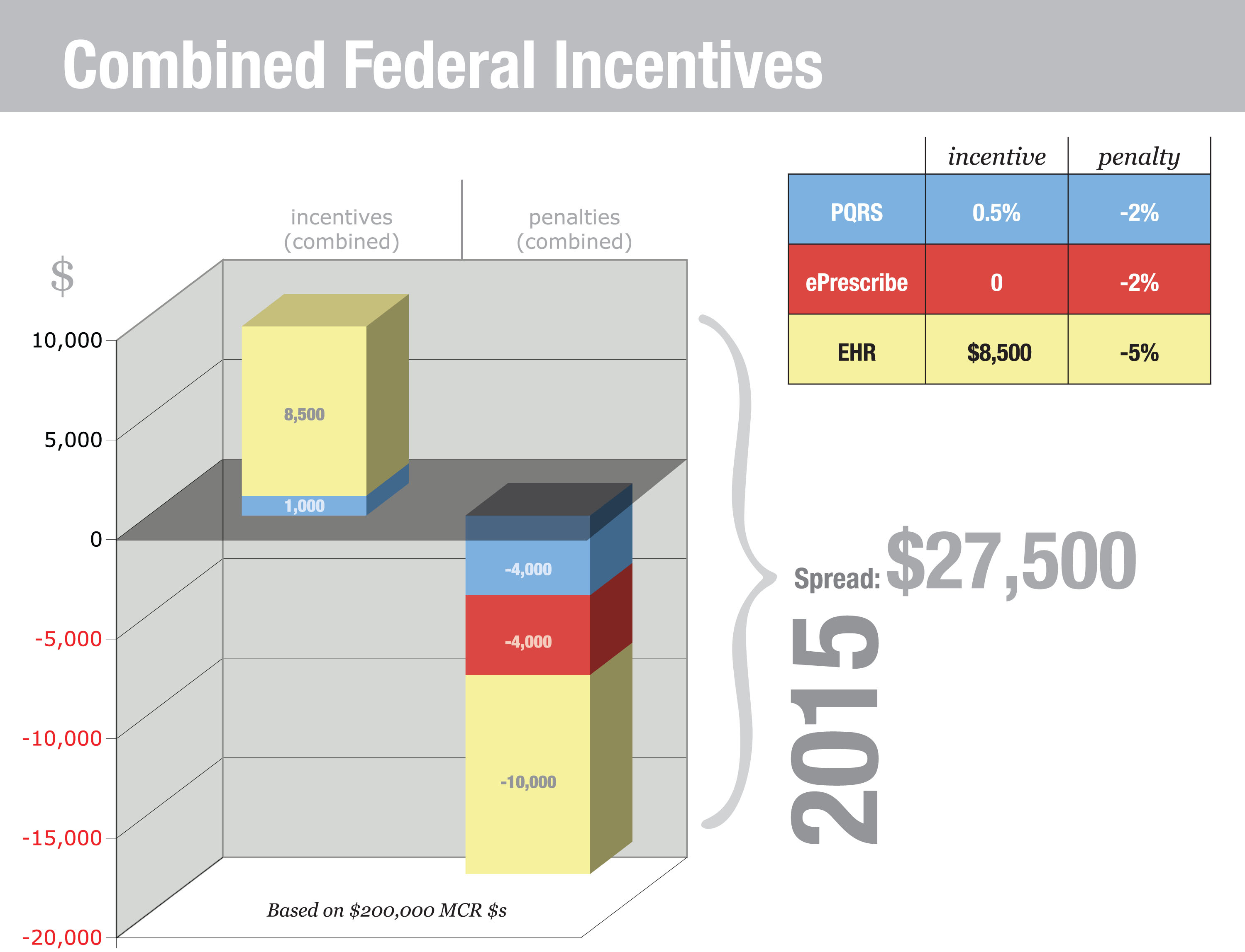
Using EHRs in Nursing Homes: Avoiding Unnecessary PainBy Rod Baird, MS Physicians must adopt certified EHR technology and demonstrate meaningful use before October 1, 2014, or face a 1% reduction in Medicare reimbursement in 2015—but there are several obstacles. Existing federal regulations require physicians and hospitals to use certified electronic medical record (EMR)/electronic health record (EHR) technology or face penalties. Many long term and post-acute care (LTPAC) facilities are implementing EHR applications knowing that the Centers for Medicare & Medicaid Services (CMS) is destined to extend the requirements. There are compelling reasons for the CMS and everyone treating the LTPAC population to embrace the use of health information technology (HIT). These patients, whether short or long term, populate the most expensive 10% of all Medicare/Medicaid beneficiaries. Unfortunately, the implementation of LTPAC HIT can have unintended consequences. Nursing homes and other LTPAC providers are not organized like hospitals or physician offices. These locations usually have patient care delivered by a closed medical staff that works more or less exclusively in a single location. Most LTPAC providers have attending medical staff members who work in multiple locations. Further, that staff of physicians and extenders is regulated by the CMS and the respective states as a medical office, and the staff members are expected to manage patient care and documentation based on that principle. To my knowledge, no existing LTPAC software meets the regulatory reporting requirements for ambulatory physicians, and most are disinterested in the physician as a customer. Many treat physicians as data entry technicians. This article attempts to build a bridge of understanding between the LTPAC facility community, software vendors, and the medical groups that treat the shared patient population. A Road Map for the LTC PCMH In a PCMH, the patient and a physician-led team take joint responsibility for a patient’s health. In an LTC PCMH, the responsibility for care shifts toward the clinical team as the patient experiences increasing cognitive deficits. The “home” of PCMH is Community Care of North Carolina, which contracts with our LTC medical group to deliver primary care to approximately 1,000 nursing facility patients as part of the first CMS Shared Savings project (the 646 program). My study for road mapping the LTC PCMH began from the perspective of an LTC medical group, the practices that increasingly provide direct patient care in the nation’s 16,100 nursing homes. Our team already understood some of the existing roadblocks to fully realizing the expectations of EHR technology for physicians practicing in the skilled nursing, nursing, or assisted-living settings. Under the aegis of Community Care of North Carolina, we had tried to implement a compliant electronic prescribing (ePrescribing) demonstration in 2011 with a national LTC chain and its LTC pharmacy partner, both in the top five national providers by size. That effort failed, for reasons that are discussed in this article. Let’s begin by framing the basic problem. From a medical record perspective, each resident is three patients: the facility’s, the attending physician’s, and the LTC pharmacy’s. All three providers are regulated, and each must answer to a set of policies and procedures mandated without consideration of respective needs in a “shared” electronic record environment. To validate the preceding statement, it is necessary to consider only the EHR ePrescribing Measure. LTC physicians are required to demonstrate use of certified EHR technology no later than October 1, 2014, or face a reduction in Medicare payments in 2015. The reduction is 1% in 2015 and increases annually to a maximum of 5%. Performance standards (core measures) require physicians to use certified ePrescribing for at least 40% of their eligible prescriptions, and their prescription messages must use National Council for Prescription Drug Programs (NCPDP) script standards. CMS regulations for LTC facilities and pharmacies exempt them from using these same NCPDP standards until November 1, 2014. It is important that facilities, pharmacies, and their respective software vendors understand the specific regulatory and legal imperatives that govern physician practices. Without an appreciation of this, unnecessary conflicts arise that may threaten the availability of an increasingly scarce resource: experienced primary care physicians and extenders. The Physician EHR Requirements In LTPAC settings, only attending physicians must comply with detailed specifications for EHR use, and they face penalties if they fail to use those records in accordance with meaningful use specification. Below is a partial list of considerations from the physician’s perspective: • EHR (HITECH Act) standards and regulations: Physicians must adopt certified EHR technology and demonstrate meaningful use before October 1, 2014, or face a 1% reduction in Medicare reimbursement in 2015. The major hurdle is ePrescribing—40% of all prescribed medications must be transmitted using a certified ePrescribing application. • Statutory requirements to report on a series of PQRS measures: This is possible using paper records, but the entire process is designed around using an EHR. The rules for PQRS reporting are highly specific, and it is doubtful a general purpose facility record would include the required measures. Failure to report successfully results in a 1.5% payment adjustment in 2014 and 2% in subsequent years. The physician must report on a defined group of patients. This must occur for more than 50% of all eligible patients, so it is unlikely this requirement would be met unless the physician has control over the EHR application and the ability to consistently select three of the 202 available measures. • ePrescribing (stand-alone quality program separate from the EHR requirement to ePrescribe): A second CMS/Medicare program exists. This could be satisfied if providers are successful EHR meaningful users, but those who aren’t incur penalties (as of 2012) unless the provider ePrescribes 10 times prior to July 1 of each year. The penalty for nonperformance is 1.5%. A small incentive (0.5%) is available for those who perform 25 instances of ePrescribing by December 31 of each year. The penalties began with this program and continue. Providers who failed to satisfy those performance levels or successfully request a hardship exemption in 2012 are already experiencing lower reimbursement payments. For the 2013 version of this program, the penalty for nonperformance has been raised to 2%. • Ownership of medical records: Under state medical board regulations, CMS reimbursement rules, and tort law, physicians are required to maintain a clinical record for each patient for whom they provide care. This record must be produced on demand. If the physician’s only record is maintained at the facility, subject to facility control, the physician may be unable to produce legally required documents on demand. There are several examples of physician groups subject to CMS claims audits that were required to make audit repayments because the facility could not retrieve archived copies of records. • Physician billing and reporting ePrescribing and PQRS data: Physician EHRs generate the complex data files necessary to support claims submission that satisfactorily reports CPT II codes for ePrescribing and PQRS measures. (This is much like reporting Minimum Data Set (MDS) 3.0 data—nearly impossible if data are gathered manually). Without a physician-centric EHR that generates claims data, this becomes a significant difficulty for attending physicians. Combined, physicians who do not have access to and control over certified EHR technology are subject to significant Medicare payment losses (see related charts 2013 and 2015 penalties). A full-time physician working in LTC most likely will generate $250,000 in allowable Medicare Part B charges. Based on that revenue, the graphics “Combined Federal Incentives 2013 and 2015” illustrate the overall income impact from the combined incentive/penalty programs (see below). Facility EHR Requirements In reality, passing ONC certification isn’t an insurmountable barrier. Receiving approval from the Certification Commission for Health Information Technology for LTPAC software is more rigorous than meeting the ONC standards. The underlying issue isn’t certification, although that is a fundamental requirement; it is workflow. LTPAC facility software evolved to address federal and state compliance mandates of conditions of participation, MDS reporting, and documentation required to support billing and audits. Touching all of these bases is an art form in itself. Great software programs allow staff to address several issues at the same time and support a naturally efficient workflow. Great software for the nursing home or home health agency is not designed around the documentation needs of the LTPAC physician or extender. The entire concept is different. Facility software is built around the incredibly detailed CMS Survey & Certification process in which exactitude in detail is paramount. Successful physician EHR applications focus on efficient workflows. Physician EHR developers spend tens of thousands of hours refining physician-specific workflows. This isn’t to diminish the importance of efficiency in either type of application but to illustrate how important usability is to the physician. Why? It’s the economics. It’s a simple fact: Physicians are the most costly health care staff in the building. It’s a rare market where a full-time primary care physician doesn’t earn a $160,000 salary plus benefits. Nurse practitioners and physician assistants are paid $80,000 or more, depending on the local market. The market determines the value of these professionals based on their unique ability to perform two functions: generate fee-for-service revenue ($50 to $200-plus per hour, depending on efficiency) and order/approve all other health services (institutional, professional, and pharmaceutical). Why would anyone want to take this very expensive and scarce resource, one that generates revenue, and require it to perform detailed order entry? The appropriate role for physicians and extenders is to review and approve orders in the facility’s EHR. Order entry in LTPAC settings is highly structured so it conforms to CMS regulations, issues of secondary concern to the attending physician. Better for a trained nurse or pharmacy tech to post the physician’s verbal orders and have the physician perform online review and approval. Expediting Workflow Successful LTC physicians and extenders regularly make themselves available by phone or in person. While it is reasonable to expect a provider to answer a call or write a brief order in the hall, expecting him or her to stop daily routines to log in to the facility EHR and enter a complete and compliant order is a massive burden and misuse of valuable time. The logical solution is to have the nurse and physician agree on an order, the nurse enter the order, and then have the facility’s EMR/EHR contact the physician electronically when an order is ready for review and approval. The NCPDP workgroup on LTPAC ePrescribing developed a model of that process for ordering medications on a newly admitted patient (see “Long-Term and Post-Acute Care/Medication Order” graphic below). This simplified workflow illustrates the key principles of a shared record. The triggering event is a phone call to the physician from the facility nurse. The physician generates a verbal order, which the nurse enters into the facility system. The message is transmitted to either the physician or pharmacy. The graphic shows a pharmacist prereview, which is particularly important in trying to adhere to multiple Part D formularies. This model is consistent with existing CMS regulations for using ambulatory EHRs and for facility-based order management. Shared Records: Are HIEs a Solution? The facility, pharmacy, and physician must share a patient’s care at each change in condition and orders. This can be a daily (or more frequent) exchange during the beginning of a Part A stay and at least monthly for the most stable patients. Patients with DEA-regulated medications present an even more pressing need for secure coordinated messaging. Messages are patient specific and need to interface directly with each provider’s records. Addressing these multiple challenges is daunting. In 2011, as an offshoot of earlier experiments, our team formed an alliance with a small group of facilities, pharmacies, and software vendors to pilot a collaborative solution. This group is migrating toward the concept of cloud-based computerized physician order entry (CPOE). This is an application developed by anyone in the LTC sphere that hosts a standard order entry system that complies with ONC standards and S & I Framework specifications. Shared Records’ Economic and Regulatory Benefits • Facility nurses record telephone orders directly into the CPOE system. This creates an opportunity to prompt the physician or nurse practitioner for elaboration when required. • Physicians using shared CPOE approve orders electronically. No more lost paperwork. • Reduced accounts receivable. There is no argument; electronic orders are signed faster. A correctly designed system forces the use of complete diagnoses prior to the physician signature. • Reduced instances of nonformulary medication use. Depending on order routing, the LTC pharmacist can review pending medication orders for nonformulary meds. • Big benefits from ePrescribing for controlled substances. While it adds costs, a CPOE system can be certified for creating electronic controlled substance prescriptions, helping to eliminate one of the most vexing compliance problems in LTC and significantly speeding up the delivery of pain management drugs. • Manage and reduce use of antipsychotic medications. Why does the CMS thrash facilities for using antipsychotic medications? Only physicians and extenders prescribe. Prescriber contracts with the facility can specify acceptance of prescribing controls. Ordering of medication classes can be restricted in the absence of documented patient need. Electronic medication orders also enable the facility medical director to better monitor staff prescribing behavior as it happens. • Bundled payments and shared savings. The CMS is driving payment reform, and LTC patients are the most costly. Shared CPOE can enable the use of order sets that are proven to reduce rehospitalizations. Time Is Not Our Ally Our only path to success lies in fostering a concurrent exchange of clinical information and authorization messages among the many providers sharing care for an LTPAC patient. It’s only at that point that any hope of constructive patient/family engagement becomes possible. The strategies proposed in this article aren’t the only possible solutions, just the only ones that my colleagues and I have identified as providing a degree of benefit to everyone. If you concur, we encourage you to begin discussions with your software vendors, professional associations, and the CMS. — Rod Baird, MS, is cofounder and president of Geriatric Practice Management based in Asheville, North Carolina.
|